Navigating the Complex Path to Nicotine Addiction Recovery
summary
Nicotine addiction recovery is a multifaceted process that involves overcoming dependence on nicotine, a highly addictive substance found in tobacco products. Recognized as a chronic brain disorder, nicotine addiction is characterized by compulsive use, repeated attempts to quit, and high rates of relapse. The addictive nature of nicotine stems from neuroadaptations in brain regions such as the amygdala and nucleus accumbens, which are disrupted during withdrawal, leading to dysphoria and anxiety. The public health implications of nicotine addiction are profound, as it is a primary cause of smoking-related diseases and mortality worldwide, prompting global efforts to address this critical issue.[1][2]
The recovery journey from nicotine addiction is unique to each individual, involving both physiological and psychological challenges. Upon cessation, the brain begins to readjust its dopamine production and receptor activity, with complete neural adjustment potentially taking months to years. Behavioral therapies, such as Cognitive Behavioral Therapy (CBT) and Motivational Interviewing, are integral in addressing the psychological aspects of addiction. Mindfulness-based interventions have also shown promise in reducing stress and anxiety during the recovery process. Emerging fields like precision medicine offer the potential for personalized treatments tailored to individual characteristics, enhancing the efficacy of recovery efforts.[3][4]
Treatment options for nicotine addiction are diverse and typically involve a combination of pharmacotherapies and behavioral therapies. Nicotine Replacement Therapy (NRT), along with medications such as bupropion and varenicline, are commonly used to alleviate withdrawal symptoms and reduce the urge to smoke. Behavioral interventions, including CBT and mindfulness-based approaches, aim to modify smoking-related behaviors and develop coping strategies to prevent relapse. Research indicates that integrated approaches, combining pharmacotherapy with behavioral support, yield higher success rates than single-method treatments.[5][6]
Public health policies and community support systems are vital components of nicotine addiction recovery. Initiatives like the Framework Convention on Tobacco Control (FCTC) emphasize the integration of smoking cessation treatments into primary healthcare services. Community-driven support networks provide essential emotional and practical resources, significantly enhancing recovery outcomes. Programs such as the Truth Initiative's EX ' Program exemplify the impact of structured digital interventions, offering personalized quit plans and support resources. The ongoing research and development in this field continue to evolve, focusing on innovative treatments and technologies to support individuals in their journey to overcome nicotine addiction.[7][8]
Understanding Nicotine Addiction
Nicotine addiction is a multifaceted condition arising from a combination of factors related to the pharmacology of nicotine and the user's biological, psychological, sociological, and environmental contexts[1]. This addiction is recognized as a chronic, compulsive brain disorder characterized by repeated efforts to quit and high rates of relapse[2]. Despite its euphoric and cognitive-enhancing effects, which contribute to the initiation of smoking, nicotine addiction is primarily sustained due to the dysphoria and anxiety associated with withdrawal, leading to frequent relapses[3].
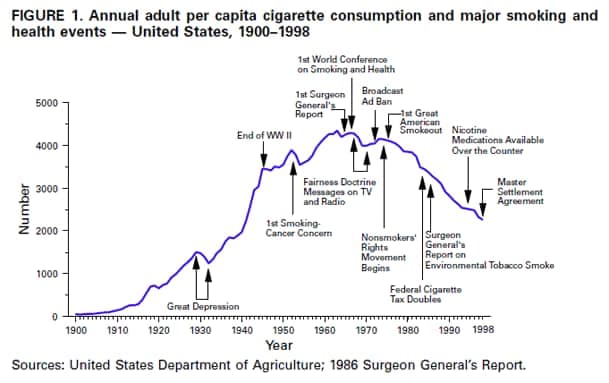
The addictive properties of nicotine have long been denied by the tobacco industry, but it is now acknowledged as a significant public health concern[1]. Nicotine is the proximate cause of disease and death resulting from cigarette smoking, making it a leading cause of mortality worldwide[4][5]. The addictive nature of nicotine is due to neuroadaptations that occur in various brain sites, such as the amygdala, nucleus of the stria terminalis, and nucleus accumbens, disrupting neurotransmitter and neuropeptide systems during nicotine withdrawal[6].
Efforts to address nicotine addiction often involve pharmacotherapy, with nicotine replacement therapy (NRT) being a prominent option. NRT is considered safe and effective, increasing the probability of cessation by 50% to 70%[2]. Beyond pharmacotherapy, mindfulness-based approaches have been studied for their potential to reduce stress, anxiety, and enhance mood during smoking cessation efforts[7]. Dispositional mindfulness, in particular, has been associated with lower levels of anger and sadness, although the role of positive emotions in this context remains unclear[8].
Recovery Process
Recovery from nicotine addiction is a complex journey that varies significantly from one individual to another. Upon quitting nicotine, the brain begins to recalibrate its dopamine production and receptor activity, showing signs of recovery within a few weeks[9]. However, complete neural adjustment can take several months to years, as the brain compensates for the absence of nicotine[9].
Counseling and behavioral therapies are integral to the recovery process, targeting the psychological and behavioral components of nicotine addiction[10]. Techniques such as Motivational Interviewing, Cognitive-Behavioral Therapy, and Contingency Management are commonly employed to equip individuals with the necessary skills and support to overcome nicotine dependence[10]. Mindfulness-based treatments have also been found to yield positive changes in mental health, including reduced stress and anxiety, which are crucial during the recovery process[7].
The withdrawal process presents both physiological and psychological challenges, demanding grit and determination from individuals seeking recovery[11]. Techniques to manage stress and cope with cravings are essential, as is the preparation for quit days and the use of tools like nicotine patches[12]. Additionally, enlisting social support and managing nutrition can help individuals navigate the multifaceted challenges of nicotine withdrawal[12].
Emerging fields such as precision medicine hold promise for nicotine addiction treatment by tailoring medical interventions to an individual's specific characteristics and needs[13]. This approach, combined with existing evidence-based resources, provides a comprehensive support system for those undergoing recovery from nicotine addiction[14].
Moreover, policy leadership and community engagement play a critical role in supporting recovery by advancing impactful policies that reduce youth access to nicotine, combat illegal e-cigarette markets, and increase access to cessation services[15]. These collective efforts ensure a supportive environment for individuals seeking to overcome nicotine addiction.
Treatment Options
There are a variety of effective treatment options available for those seeking to overcome nicotine addiction, which can be broadly categorized into behavioral therapies and pharmacotherapies. Research suggests that a combination of these treatments often results in higher success rates for smoking cessation than using one method alone[16][17].
Behavioral Therapies
Behavioral therapies aim to modify smoking-related behaviors and develop skills to avoid triggers that prompt smoking. Cognitive Behavioral Therapy (CBT) is one of the most effective interventions, helping individuals recognize and restructure thought processes and develop new coping strategies for relapse prevention[18][19]. CBT's structured approach has been empirically supported for various psychological disorders, including addiction, by helping patients identify triggers and teaching them relaxation techniques and coping strategies[20][19].
Mindfulness-based interventions (MBIs) are another promising approach for treating nicotine addiction. These interventions combine traditional addiction treatments with mindfulness practices such as meditation and yoga, which foster self-awareness and focus on the present moment[21][22]. MBIs have been applied successfully across a range of addictions and help reduce dependence, craving, and improve mood regulation[23][24].
Pharmacotherapies
Pharmacotherapies approved by the FDA include various forms of nicotine replacement therapy (NRT), such as patches, gums, and lozenges, as well as medications like bupropion and varenicline[16][25]. These treatments are designed to alleviate withdrawal symptoms and reduce the urge to smoke by delivering controlled amounts of nicotine without the harmful effects of tobacco. NRT is considered safe and can increase the probability of cessation by 50% to 70%[2].
Advancements in medication development have led to innovative treatments, such as allosteric modulators at addiction-relevant targets, which display better target specificity and fewer adverse side effects compared to traditional agonists and antagonists[26]. Additionally, the field is exploring the application of precision medicine and new technologies to deliver support in real-time, aiming to further enhance the effectiveness of these pharmacotherapies[27][28].
Integrated Approaches
Combining behavioral therapies with pharmacotherapies is generally more effective than using either approach alone[16]. For instance, integrating CBT with contingency management (CM), which provides tangible rewards for maintaining abstinence, has shown higher treatment retention and abstinence rates compared to CBT alone[29]. Health care providers are also encouraged to address social determinants of health as part of a comprehensive treatment and recovery plan for nicotine addiction[30].
Self-Help Strategies
Self-help strategies play a crucial role in nicotine addiction recovery by empowering individuals to take control of their own treatment process. These strategies often include recognizing triggers, practicing stress management techniques, and preparing for quit days through structured planning[12]. One effective self-help method involves enlisting social support, which can be derived from family, friends, and peers. Studies have shown that individuals with robust support networks have a higher likelihood of overcoming addiction compared to those attempting recovery in isolation[31].
Mindfulness-based interventions are another self-help approach that has shown success in reducing dependence, craving, and other addiction-related symptoms[23]. These interventions improve mood states and help regulate emotions, contributing to a more stable recovery process. Dispositional mindfulness has been linked to lower levels of anger and sadness during smoking cessation, although the role of positive emotions in this context is still being studied[8].
Precision medicine is an emerging field that offers personalized self-help strategies by tailoring treatments to an individual's unique characteristics. Through genetic testing and other personalized approaches, precision medicine aims to identify the most effective treatment strategies for nicotine addiction, thus enhancing the self-help process[13].
Understanding the withdrawal process is also a key component of self-help strategies. From the initial hours of quitting to the eventual fading of withdrawal symptoms, individuals must navigate both physiological and psychological challenges[11]. By combining behavioral economics insights with engagement in drug-free social behaviors, self-help strategies can significantly reduce alcohol use and increase participation in rewarding, drug-free activities[32].
Support Systems
Support systems play a crucial role in nicotine addiction recovery, providing both formal and informal avenues of assistance that can significantly enhance the chances of successful cessation. These systems range from structured support groups and rehabilitation programs to the informal support offered by family, friends, and peers[31]. Research indicates that individuals with strong support networks are more likely to overcome addiction than those attempting recovery independently[31].
Community support not only facilitates recovery from nicotine addiction but also positively impacts mental health by reducing anxiety, depression, and loneliness, which are common among those battling addiction[33]. The interconnectedness within these groups underscores the importance of incorporating community support into recovery programs[33].
A notable example of effective community support can be seen in recovery high schools (RHS), which separate students undergoing recovery from traditional high school environments. These schools offer peer support groups and access to staff with expertise in drug use recovery, resulting in increased abstinence self-efficacy among students[34]. Moreover, the evolution of roles such as "recovery coaches" or "peer recovery specialists" highlights the growing recognition of peer-to-peer support services as an integral part of addiction treatment[34].
Support systems are also complemented by comprehensive, evidence-based resources such as the Truth Initiative's EX ' Program, which offers digital smoking cessation tools and personalized quit plans[14]. Expanding accessibility to these recovery supports and services is crucial, with diverse funding streams being advocated to sustain these initiatives[35].
Additionally, addiction hospitals are encouraged to provide structured behavioral support, integrating counseling sessions with nicotine replacement therapies or other medications to address tobacco dependence effectively[36]. This holistic approach, which includes cognitive behavior therapy and insights from social learning models, enhances the ability to cope with addiction by focusing on behavioral, cognitive, and environmental factors[20][37].
Challenges in Recovery
Recovering from nicotine addiction presents numerous challenges due to the complex interplay of psychological, behavioral, and physiological factors. One of the most formidable challenges is the intense craving or urge to smoke, which is a strong predictor of relapse[38]. This craving is often exacerbated by the mildly euphoric and cognitive-enhancing effects of nicotine, which contribute to the initiation of smoking, while the dysphoria and anxiety associated with cessation further complicate the recovery process[3].
Behavioral interventions such as Cognitive Behavioral Therapy (CBT) play a crucial role in addressing these challenges by helping individuals identify and manage triggers, such as people, places, and situations that prompt smoking[18]. CBT is designed to teach relapse-prevention skills and effective coping strategies to navigate stressful situations without resorting to smoking[18]. Despite these interventions, the social environment and personal characteristics of individuals, as well as drug-centric behaviors, can continue to pose significant barriers to recovery[32].
Pharmacological aids like nicotine replacement therapy and medications such as bupropion and varenicline are also employed to mitigate the physical dependency on nicotine. These FDA-approved treatments are used to deliver a controlled amount of nicotine to the body, reducing withdrawal symptoms while the individual works on the psychological aspects of addiction[16][39]. Research indicates that a combination of behavioral therapies and cessation medications can improve the rates of successful quitting[16].
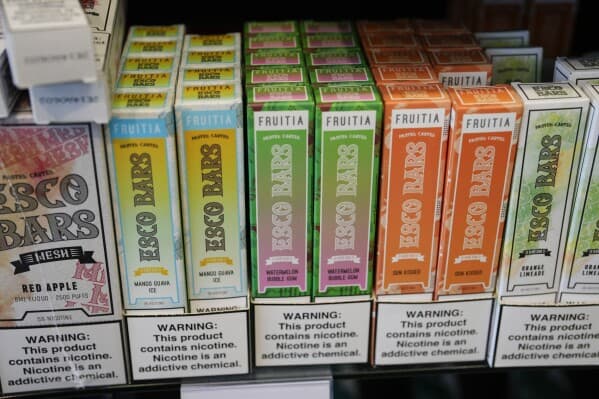
Nevertheless, the path to recovery is often hindered by the persistent social and environmental cues that trigger smoking behavior[32]. Moreover, the public health challenges related to new and emerging nicotine products complicate recovery efforts, as they sustain nicotine addiction and present a significant global health concern[40]. The process of overcoming nicotine addiction is multifaceted, requiring a comprehensive approach that addresses both the psychological and physical dimensions of addiction[10][20].
Public Health Policies and Measures
Public health policies and measures play a crucial role in addressing nicotine addiction recovery. One significant approach is the integration of smoking cessation treatments into primary healthcare services, as endorsed by over 160 countries through the Framework Convention on Tobacco Control (FCTC)[41]. This framework obliges state governments to treat tobacco dependence using various methods, ranging from simple medical advice to pharmacotherapy[41].
Efforts by federal agencies, including the Centers for Disease Control and Prevention, the Food and Drug Administration, and the Centers for Medicare and Medicaid Services, focus on preserving the Tobacco Control Act, preventing commercial tobacco use, and supporting individuals in overcoming nicotine addiction to prevent chronic diseases[42]. The proposed Framework to Support and Accelerate Smoking Cessation by the Department of Health and Human Services (HHS) is a significant step toward addressing health disparities among populations disproportionately affected by smoking-related illnesses. This framework aims to improve accessibility to culturally tailored cessation treatments and programs[43].
Moreover, the Change for Life initiative highlights the importance of integrating tobacco-use treatment into behavioral health programs, which can enhance long-term recovery prospects and improve mental health outcomes while reducing health risks associated with chronic diseases[44]. Developing new tools and expanding access to evidence-based interventions for nicotine addiction, ensuring equitable access, is central to public health goals[45].
Structured behavioral support in addiction hospitals, combining counseling sessions with nicotine replacement therapy or other medications, is crucial for effectively addressing tobacco dependence[36]. This comprehensive approach surpasses short, brief interventions, which are no longer considered sufficient[36]. Additionally, community support plays a vital role in addiction recovery. Formal and informal support networks, including family, friends, and peers, significantly enhance the likelihood of successfully overcoming addiction compared to individuals recovering in isolation[31]. These community support networks can positively impact mental health by reducing anxiety, depression, and loneliness, common challenges faced by individuals battling addiction[33].
Success Stories
Success stories in nicotine addiction recovery highlight the profound impact of structured support systems and innovative treatment approaches. Programs like the Truth Initiative's EX ' Program have been pivotal in providing comprehensive, evidence-based resources to individuals seeking to quit nicotine and tobacco use. This digital smoking cessation program offers personalized quit plans, helping participants tailor their journey to quitting based on their unique needs and circumstances[14].
In addition to structured programs, community support plays a crucial role in recovery. Local community centers often host events and programs that create a supportive environment for individuals in recovery. These community-driven initiatives offer emotional support, practical resources, and a sense of belonging, which can significantly influence successful recovery outcomes[46].
Furthermore, mindfulness-based addiction treatment (MBAT) has emerged as a successful intervention for smoking cessation. This 8-week group-based program focuses on increasing present-focused awareness of internal phenomena and developing healthier responses to challenges. Participants in MBAT have reported enhanced ability to manage thoughts and emotions related to nicotine cravings, contributing to their success in quitting[24].
Research and Developments
The field of nicotine addiction recovery is experiencing significant advancements, characterized by innovations in medication development, the adoption of precision medicine, and the integration of new technologies for support delivery in real-time and over extended periods[27]. A prominent trend in current research is the development of new nicotine and tobacco products alongside novel treatments, with a growing emphasis on person-, home-, and community-facing technologies[47].
Precision medicine is emerging as a promising approach in the treatment of nicotine addiction. This approach involves tailoring medical treatment to the individual's specific genetic makeup and needs, which may enhance the effectiveness of treatment strategies[13]. Genetic testing and personalized approaches are being explored to identify the most effective interventions for individual patients[13].
Moreover, evidence-based interventions remain central to efforts aimed at nicotine addiction recovery. A 2023 meta-analysis of Nicotine Replacement Therapies (NRTs) examined 68 studies and found that combining different NRT methods, such as nicotine gum with a nicotine patch, proved more effective than using any single method alone[48]. Higher-dose NRT products were also found to be more efficacious compared to their lower-dose counterparts, and there is evidence suggesting the benefit of using NRT prior to quitting smoking[48].
State governments, under international frameworks like the Framework Convention on Tobacco Control (FCTC), are mandated to incorporate tobacco dependence treatment into their primary healthcare services. This encompasses a range of methods, from providing simple medical advice to administering pharmacotherapy[41]. Effective public health initiatives have also been instrumental in reducing tobacco use rates in certain regions, highlighting the impact of strategic policy implementation[49].